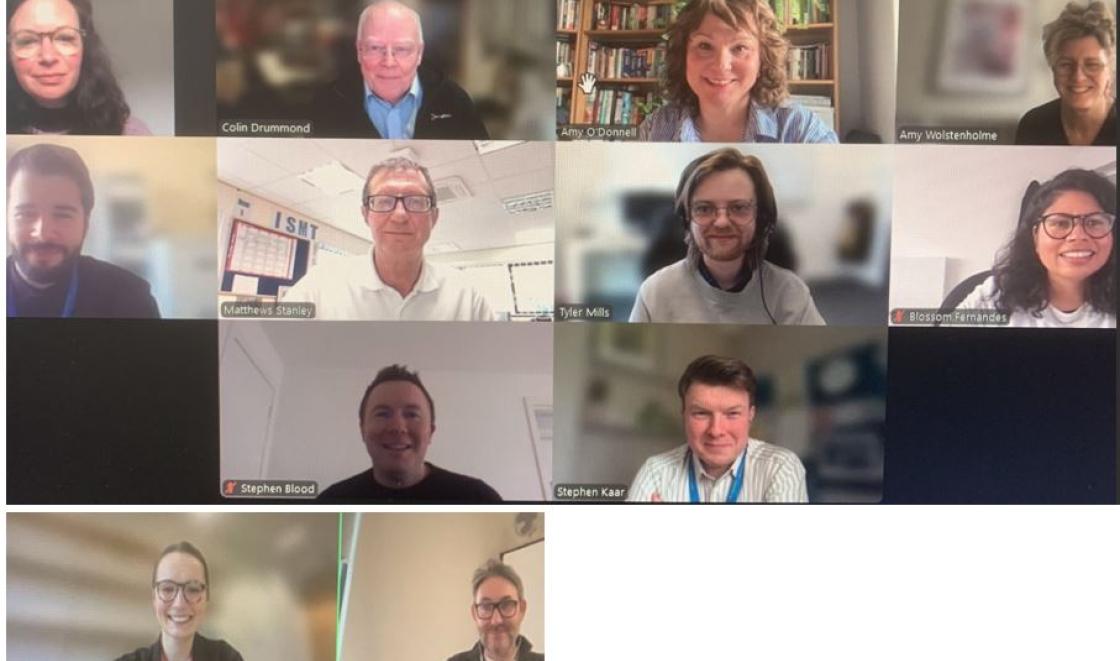
(Photo: Speakers from top row left - Kelly Davies, programme manager, Emeritus prof Colin Drummond, prof Amy O'Donnell, Amy Wolstenholme, Dr Nikos Mylonas, Stanley Matthews, Dr Tyler Mills, Dr Blossom Fernandes, Stephen Blood, Dr Stephen Kaar, Lucy Gallagher and Prof Tom Phillips.)
Around 170 mental health clinicians, practitioners, researchers, commissioners and people with lived experience of alcohol dependence co-occurring health conditions joined the webinar and discussed the challenges, outcomes, including cost savings for the local health economy, and implementation strategies for AAOT.
The webinar included:
- Experiences of implementation in Hull and Greater Manchester
- Implementation strategies and the role of Communities of Practice
- An implementation science perspective of sustainability of AAOT
- Patient and public involvement in AAOT
- Service users from London, Hull and Manchester sharing their experiences
- Development of an Alcohol Assertive Outreach Treatment Toolkit.
Colin Drummond, Emeritus Prof Addiction Psychiatry, King’s College London welcomed everyone to the event explained that the event was the culmination of six years of work and an exciting opportunity to share findings about implementing alcohol assertive outreach in three regions of England. “We hope this event will encourage you to adopt and spread the AAOT approach across England.”
A study led by Amy Wolstenhome, research fellow, King’s College London evaluated the impact of AAOT on admissions to King’s College Hospital and found that following implementation of the AAOT programme there was a 23% reduction in overall alcohol admissions to the hospital. Frequent attenders at hospital were targeted to help them find better ways of managing their health in the community. Her economic evaluation found that AAOT led to saving of £10,470 per patient per year compared to care as usual.
Research in Manchester and Hull both found that alcohol assertive outreach treatment lead to reduced emergency hospital admissions.