Our research will explore ways of reducing the morbidity associated with both disorders, using data systems to inform prevention and care. Smoking remains a significant cause of both diseases and many others. We are designing and evaluating new smoking prevention pathways in hospitals and in the community.
Aims of our research
Through our research – on diabetes, vascular disease and smoking – we aim to reduce the impact of having more than one health condition at both a population and personal level.
Diabetes – project to improve type 2 diabetes (T2D) prevention and preventive management of T2D complications in primary and secondary care
Our diabetes researchers will develop interventions to reduce the energy intake from people’s diets in order to prevent and manage T2D risks, particularly those of South Asian, African and Caribbean origin. We will then test their effectiveness and cost-effectiveness. We will also develop screening tools to identify patients at high risk of T2D complications and co- morbidity, testing algorithms in large primary care datasets and embedding them in culturally tailored models of care.
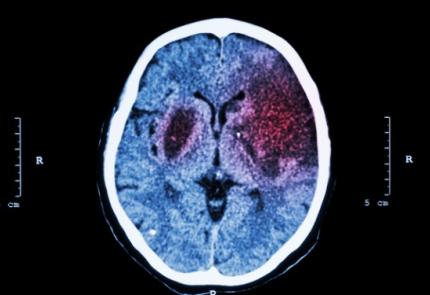
Vascular – project to use integrated data to inform delivery of prevention and care of vascular morbidities such as stroke
Our vascular researchers will analyse data to better understand the relationship between a patient’s first and subsequent vascular events, such as stroke or heart attack. They will also seek to understand better the factors that put patients at risk of vascular disease to inform health policy and service delivery.
Smoking – project to evaluate a CCG-commissioned tobacco dependence treatment pathway and to develop a tobacco dependence treatment pathway in community mental health services
Our smoking team will evaluate a tobacco dependence treatment pathway in acute medical care, which has been commissioned by a Clinical Commissioning Group (CCG). The team will create a toolkit to help local acute medicine and mental health teams to implement an integrated tobacco dependence treatment programme.
How our work is addressing multimorbidities and inequalities
Our research is targeting the patient groups at highest risks of suffering with comorbidities. We are working closely with colleagues in local authorities to ensure that cost-effective interventions are co-designed and suitable for implementing locally. This will include em- bedding a researcher within local service teams. In this role, the researcher will support public participation and explore how it might be done better in relation to mental health and youth violence.
Involving patients, services users, carers and public
We are working with local people to co-produce new population- focused health interventions to be incorporated into integrated care systems (ICSs) and local government prevention strategies. The work has started with a series of workshops involving local people, including young people. We will be working closely with the Centre for Public Engagement at St George’s, University of London.
Our collaborators
We are collaborating with researchers, health professionals, patients and members of the public locally, nationally and internationally. We have close links to public health professionals at both Lambeth and Southwark Councils, as well as NICE and Public Health England.
How are we taking this work forward
Building on our current work, we will evaluate the effectiveness of a tobacco harm reduction intervention for people in south London with multiple long-term conditions and assess smoking- and disease-specific outcomes. We are also testing the feasibility of a digital diabetes prevention intervention in women with gestational diabetes. Our vascular researchers are working on identifying the mechanisms underlying observed demographic disparities in vascular multimorbidity and related health outcomes.
Find out more
- Read a letter (March 2022) outlining findings from research assessing the fairness of decision-making at PHARMAC, a New Zealand government agency that decides which medicines to fund. The research was carried out using the Decision-Making Audit Tool (DMAT), developed under NIHR CLAHRC South London.