Addressing this gap in support for children and young people
The Mental Health Implementation Network aims to address this gap in treatment and services by supporting interventions designed to increase access to a range of psychological therapies for children and young people.
The project will build on the approach developed by the NHS’s Improving Access to Psychological Therapies (IAPT) programme. Since it began in 2008, this IAPT programme has transformed the treatment of adult anxiety disorders and depression in England – providing millions of adults with access to talking therapies to help overcome their depression and anxiety.
IAPT-style interventions could help to meet the needs of children experiencing adverse childhood experiences (ACEs) – such as neglect, poverty, losing a parent, or living with a parent with severe mental illness – and children living with their own mental health difficulties. Access to therapies can help to identify children experiencing difficulties, refer them for treatment if needed, and provide a range of support through interventions delivered at school.
Interventions delivered in school to support mental health have been shown to help build resilience and wellbeing in children, address problem behaviours, and support positive family relationships. These interventions usually include a combination of interactive educational and psychosocial-based activities delivered by teachers at a low-cost.
Aim of this project
The aim of this MHIN project is to expand access to mental health care for children and young people using IAPT-style services, especially by increasing available support in schools.
In expanding the availability of IAPT-style services, we aim to:
- Improve the resilience and wellbeing of children and young people
- Reduce behaviour problems in children and young people
- Identify children and families who need tailored support
- Reduce waiting times for children and young people from referral to treatment.
Selecting interventions for scale up
Supporting the priorities in the NHS national transformation programme, the MHIN selected an intervention to implement parent-led cognitive behavioural therapy (CBT) to help address child anxiety. They focused on two intervention sites: working with mental health support teams on the Northwest Coast and primary school support staff in the East of England to support interventions co-developed with clinicians, researchers, children and families.
Why child anxiety?
Anxiety is one of the most common mental health difficulties in childhood, with 50% of anxiety cases beginning before the age of 12. But access to evidence-based treatments is limited with long waiting lists for support. If left untreated, anxiety can severely impact social development, education attainment, and wellbeing.
Therapist-guided parent-led CBT is a brief intervention for children aged 5-12 with anxiety. It has been shown to improve access to anxiety treatments, taking less therapist time to deliver, without compromising child outcomes or parent satisfaction.
Implementing parent-led CBT to help address child anxiety
In the Working on Worries MHIN project in the East of England, primary school support staff in Norfolk were trained to help families access parent-led CBT.
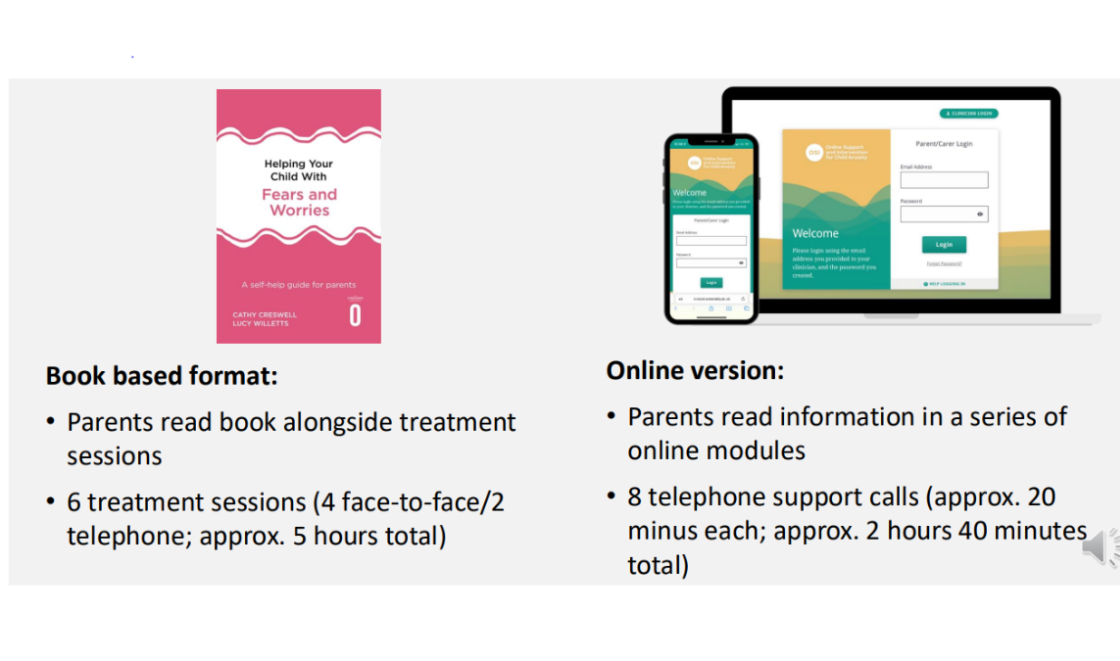
The intervention can be delivered in a book format or online (pictured below).